Vector-borne diseases: A growing menace to Nigeria's Public Health

Lagos, Nigeria - Beyond malaria, mosquitoes pose a greater threat to public health by transmitting a multitude of other life-threatening diseases, yet, many people are still in the dark about the fact that these same insects also transmit a range of other potentially fatal diseases.
This limited understanding overlooks the broader threat posed by mosquitoes, which are vectors for a variety of other life-threatening diseases such as Dengue fever, Zika virus disease, Chikungunya, and Yellow fever.
These diseases, though less publicized, are no less dangerous and continue to impact millions worldwide, particularly in tropical and subtropical regions.
Vectors are living organisms that transmit infectious pathogens between humans or from animals to humans. Many vectors are bloodsucking insects, such as mosquitoes, ticks, and flies, that ingest disease-producing microorganisms during a blood meal from an infected host.
Every year, vector-borne diseases account for more than 17% of all infectious diseases, causing over 700,000 death from diseases such as malaria, dengue, schistosomiasis, human African trypanosomiasis, leishmaniasis, Chagas disease, yellow fever, Japanese encephalitis and onchocerciasis according to World Health Organization (WHO) report.
Among the most prevalent vector-borne diseases is malaria, a parasitic infection transmitted by Anopheline mosquitoes, which causes an estimated 219 million cases globally each year and results in over 400,000 deaths, most of which occur in children under five.
Similarly, more than 3.9 billion people across 129 countries are at risk of contracting dengue, leading to an estimated 96 million symptomatic cases and 40,000 deaths annually.
Other vectors, such as aquatic snails, blackflies, sandflies, and ticks, also play significant roles in spreading diseases like schistosomiasis, onchocerciasis, leishmaniasis, and Lyme disease.
The impact of these diseases extends beyond the immediate health consequences. They contribute to high levels of morbidity, disrupt economic activities, and place a heavy burden on healthcare systems.
The Ongoing Battle Against Mosquitoes and Malaria

A sample of a mosquitoe used in illustrating the story.
According to the 2019 World Malaria Report from WHO, Nigeria bears a significant portion of the global malaria burden. The country accounted for 23% of the world's malaria deaths, with over 88,000 fatalities, and 27% of the global malaria cases, totaling over 61 million in 2019.
This has led to an intensified malaria prevention and control efforts in Nigeria, as the disease remains a major public health challenge with devastating impacts on the population, particularly among children under five and other vulnerable groups.
Mosquitoes remain one of the deadliest animal on the planet, responsible for killing more people annually than any other creature.
Among the diseases they spread, malaria is one of the most devastating, particularly in sub-Saharan Africa, where it remains the leading cause of outpatient visits, work and school absenteeism, and a major contributor to under-five mortality according to the International Society for Infectious Diseases (ISID).
ISID highlighted that majority of malaria cases and deaths occur in low-resource settings. These regions are disproportionately affected by the disease's morbidity and mortality due to limited access to preventive measures, timely diagnosis, and effective treatment.

For malaria, WHO recommends two key vector control interventions: indoor residual spraying (IRS) and insecticide-treated nets (ITNs). Insecticide-treated nets provide a physical barrier that protects individuals from mosquito bites while they sleep, significantly reducing the risk of infection.
Meanwhile, indoor residual spraying involves the application of insecticides on the interior walls of homes and other buildings where disease-transmitting mosquitoes are likely to rest.
This method not only kills Anopheles mosquitoes but can also be effective against other disease-carrying insects.
However, the effectiveness of these interventions is contingent on equitable access.
Dengue fever: A Growing Global Threat on Public Health
According to WHO, dengue is a viral infection transmitted to humans through the bite of infected Aedes mosquitoes.
The disease is now endemic in more than 100 countries, with Africa, the Americas, South-East Asia, and the Western Pacific regions being the most seriously affected. Often referred to as “break-bone fever” due to the severe joint and muscle pains it causes, dengue is most common in tropical and subtropical climates.
It has become an increasing concern, particularly as it spreads to new regions and infects millions each year.
In December 2023, the Nigeria Centre for Disease Control and Prevention (NCDC) confirmed an outbreak of dengue fever in Sokoto State, initially reported in November 2023.
The report shows that 71 suspected cases were identified, with 13 confirmed through laboratory testing.
The virus was detected in three local government areas (LGAs): Sokoto South, Wamako, and Dange Shuni, with Sokoto South recording the highest number of cases at 60.
The majority of the suspected cases fall within the age range of 21-40 years, indicating that this demographic may be particularly susceptible in the outbreak. The NCDC, in collaboration with its multisectoral partners through the National Emerging Viral Haemorrhagic Diseases Technical Working Group (NEVHD-TWG), conducted a rapid risk assessment to guide the preparedness and response activities in the affected regions.
According to a report in the National Library of Medicine, recent studies indicate that dengue viruses are emerging as a significant cause of acute fevers in Nigeria. Seroprevalence surveys conducted in Maiduguri (Northern Nigeria) and Ilorin (Western Nigeria) revealed that 10.1% and 30.8% of participants, respectively, tested positive for dengue subtype-3 virus (DENV-3).
The report showed that in South-Western Nigeria, dengue IgM seroprevalence among febrile children has been reported to be 17.2% and 30.8%. These high prevalence rates of symptomatic dengue infections and IgM antibodies suggest that dengue could be becoming endemic in Nigeria, with many cases potentially being missed by frontline health workers.
Additionally, there is evidence of high vector density in densely populated Nigerian cities, further indicating that dengue is an increasing public health concern in the country. The situation is complicated by the high rates of co-infection with malaria and dengue.
A recent report from Ibadan, South-Western Nigeria, revealed that 10% of confirmed malaria cases also had active dengue co-infection. These findings underscore the need for more focused attention on dengue in Nigeria, as its true magnitude remains underexplored.
While many dengue infections are asymptomatic or cause only mild illness, the virus can occasionally lead to severe cases and even death, particularly in individuals who have been previously infected with a different strain of the virus. Most people infected with dengue will experience mild or no symptoms and will recover within 1–2 weeks.
However, symptoms that do appear usually begin 4–10 days after infection and can include high fever, severe headache, pain behind the eyes, muscle and joint pains, nausea, vomiting, swollen glands, and a rash. In severe cases, dengue can lead to life-threatening conditions such as severe abdominal pain, persistent vomiting, rapid breathing, and bleeding gums or nose.
WHO reports that there is currently no specific treatment for dengue or severe dengue. Management of the disease primarily involves relieving symptoms with pain relievers such as acetaminophen (paracetamol) and ensuring that patients stay hydrated. Early detection and access to proper medical care greatly reduce fatality rates in severe dengue cases.
Yellow Fever: A High-Threat Disease with Global Health Implications
Yellow fever, a mosquito-borne disease, continues to pose a significant threat to global health security, especially to countries in Africa and the Americas. Research shows that, the Aedes and Haemagogus mosquitoes that spread yellow fever are day-biters and breed in various environments, including domestic areas around houses, forests, jungles, and semi-domestic habitats.
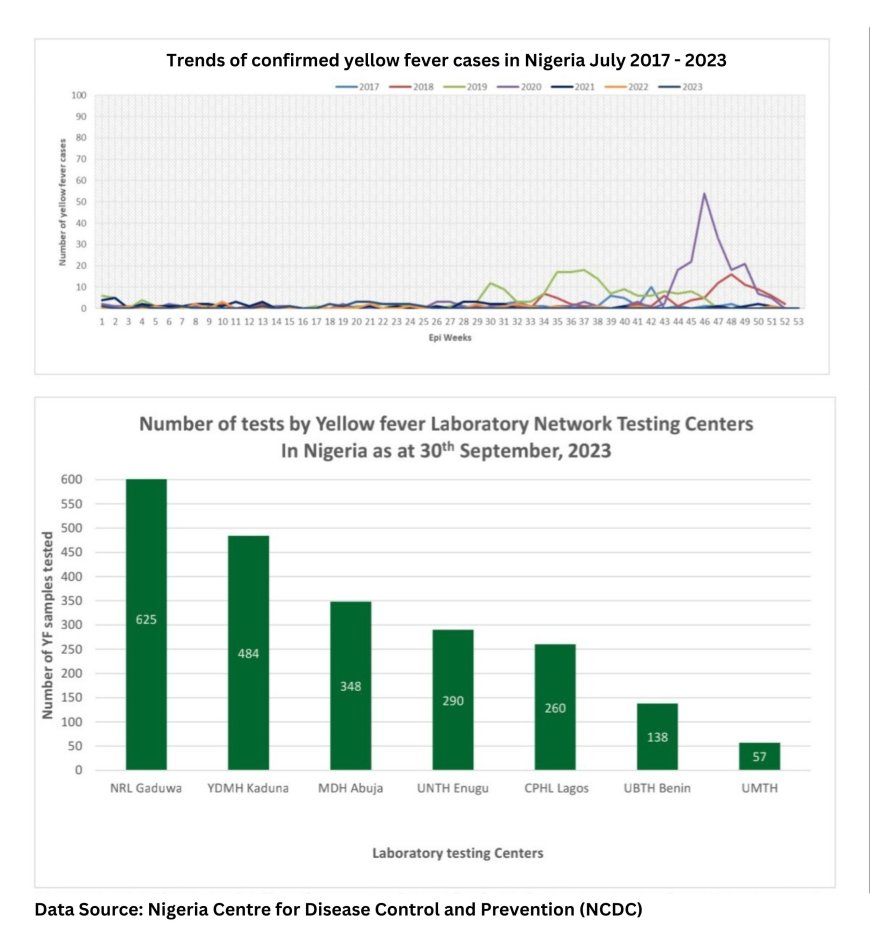
Map showing yellow fever trends in Nigeria
According to a Yellow Fever situation report by NCDC, from January 1 to September 30, 2023, a total of 2,203 suspected cases were reported across 492 Local Government Areas (LGAs) in 36 states, including the Federal Capital Territory (FCT).
The reported cases were distributed among various states: Abia (28), Adamawa (12), Akwa Ibom (9), Anambra (77), Bauchi (326), Bayelsa (39), Benue (54), Borno (157), Cross River (37), Delta (14), Ebonyi (16), Edo (26), Ekiti (34), Enugu (116), FCT (19), Gombe (4), Imo (55), Jigawa (107), Kaduna (26), Kano (17), Katsina (190), Kebbi (85), Kogi (34), Kwara (37), Lagos (14), Nasarawa (47), Niger (97), Ogun (63), Ondo (79), Osun (19), Oyo (51), Plateau (80), Rivers (18), Sokoto (36), Taraba (112), Yobe (40), and Zamfara (28).
The gender distribution showed 1,157 males (52.5%) and 1,046 females (47.4%) among the suspected cases. Notably, 76% of the cases occurred in individuals aged 30 years and below. Out of the 2,203 suspected cases, 213 individuals (9.7%) had received at least one dose of the yellow fever vaccine.
Similarly, data from WHO report shows that since September 2017, yellow fever cases have been reported across several states in Nigeria. From January 1 to August 31, 2021, a total of 1,312 suspected cases were documented in 367 Local Government Areas (LGAs) across 36 states and the Federal Capital Territory (FCT).

Map showing areas with Risk of Yellow Fever in Africa [Source: U.S Centre for Disease Control and Prevention (CDC)]
During this period, 45 blood samples were sent to Institut Pasteur in Dakar (IPD), and 31 samples tested positive for yellow fever through the Plaque Reduction Neutralization Test (PRNT). Of these 31 PRNT-positive cases, twelve had a history of yellow fever vaccination. Unfortunately, two deaths were reported among the 19 non-vaccinated PRNT-positive cases, resulting in a case fatality ratio of 11%. These 19 cases were reported from Enugu (7), Anambra (3), Benue (3), Delta (2), Oyo (2), Niger (1), and Osun (1).
Nigeria has identified significant gaps in population immunity against yellow fever. In a 2020 UNICEF estimates, the national immunization coverage for yellow fever was 54%, which is below the 80% threshold necessary to prevent outbreaks. In the nine states reporting PRNT-positive cases, routine immunization coverage declined between 2018 and 2020, falling below 80% in 2020. These states include Anambra, Benue, Delta, Enugu, Imo, Niger, Ondo, Osun, and Oyo, with six states reporting coverage below 50% (Anambra, Delta, Enugu, Imo, Osun, and Oyo).
Knowledge Gap Puts Residents at Risk
In a series of interviews with residents in Lagos state, Nigeria, many believed that mosquitoes are solely responsible for spreading malaria, a perception largely shaped by the intense global efforts and awareness campaigns focused on eradicating the disease.
In a visit to Ketu market, Mrs. Adebayo Yinka, expressed her surprise at the broader threat posed by mosquitoes, stating, "I've always known mosquitoes cause malaria, but I didn't realize they could spread other serious diseases too. Malaria is what we've been taught to fear, but now I'm hearing about dengue and Zika. It's worrying because we don't have much information about those diseases here."
Similarly, Mr. Chinedu Emmanuel, in Mile 12 Market, shared his experience with a lesser-known mosquito-borne disease: "We are used to dealing with malaria, but I was shocked when my nephew was diagnosed with yellow fever after a visit to the village. We had no idea mosquitoes could cause something so different from malaria. It’s clear we need more education about these other diseases."
Fatima Ireti, a student, highlighted the gaps in public health education, noting, "Most people I know only associate mosquitoes with malaria. Even in school, we mainly learned about malaria prevention, but there's little discussion about other diseases like the Zika or yellow fever. It’s as if malaria is the only thing mosquitoes can cause.”
Mr. Ibrahim Ojo, a civil servant, recounted a troubling encounter with an unfamiliar illness: “You see that Salah period, I travelled home to my hometown in Ogun state, in my community, malaria is a common problem that everyone knows, but when my neighbour fell ill with severe joint pain, we thought it was just a case of the farm work and all that. It turned out to be yellow fever. I was so surprised when I heard it from the wife. It made me realize how much we don't know about the dangers mosquitoes can bring.”
In a visit to some secondary schools in Kosofe Local Government Area, many students were not aware of the full range of diseases transmitted by mosquitoes. While most were familiar with malaria and its prevention, they had limited knowledge about other serious mosquito-borne illnesses such as dengue, yellow fever, Zika, and chikungunya.
Mrs. Nneka Amadi, a secondary school teacher, emphasized the need for broader awareness: "We’ve been taught to use nets and sprays to protect against malaria, but I never knew mosquitoes transmit diseases like Zika. It’s scary because we’re not equipped to handle those. There should be more awareness campaigns so people understand all the risks, not just malaria."
Expert Highlights Key Challenges on the Fight Against Mosquito-borne Diseases in Nigeria
Bukola Christiana Okusanya, a Public Health expert, shed light on the critical obstacles hindering the fight against mosquito-borne diseases especially in Nigeria. Okusanya emphasized that issues such as poor sanitation, inadequate drainage, and ineffective mosquito control measures are exacerbating the spread of these illnesses in many households.

Residents neglect environment with less concern about sanitation posing high risk for a breeding ground for mosquitoes and other vectors in Alapere, Lagos State, Nigeria
She explained that poor sanitation and waste management create breeding sites for mosquitoes due to improper disposal of waste and debris. "Inadequate drainage systems are another issue," Okusanya noted. "Clogged or non-existent drains lead to standing water, which is ideal for mosquito breeding."
She also pointed out that a lack of access to clean water forces people to store water in containers, providing additional breeding grounds for mosquitoes. "Ineffective mosquito control measures are a significant problem as well," she added. "When insecticides and nets are not properly implemented or maintained, mosquito populations can thrive."
Okusanya highlighted the role of limited public awareness and education, saying, "Insufficient knowledge about mosquito-borne diseases and prevention methods hinders efforts to control outbreaks." She also shared that insufficient healthcare resources impede the diagnosis, treatment, and management of these diseases. She further addressed the impact of climate change, noting that altered temperature and precipitation patterns are changing mosquito habitats and behaviour, which increases disease transmission.
Behavioural Changes and the Risk of Mosquito-Borne Diseases in Nigeria
Okusanya outlined key habits that can increase the risk of mosquito-borne diseases and called for critical behavioural changes. She stressed that neglecting to use insecticide-treated nets, not wearing protective clothing, and failing to apply insect repellents significantly heightens vulnerability to mosquito bites.
"Failing to use treated bed nets is a major oversight in protecting yourself from mosquito-borne illnesses," she emphasized. She also noted the importance of wearing protective clothing, stating, "Not wearing long sleeves, pants, and closed shoes when outdoors makes you more vulnerable to mosquito bites."
She highlighted the significance of applying insect repellents, saying, "Not using repellents containing DEET, Picaridin, or oil of lemon eucalyptus leaves you unprotected against mosquito bites." She stressed the need to address standing water around homes, noting, "Allowing water to collect in containers, gutters, or yards creates ideal breeding sites for mosquitoes."
She also pointed out the risks associated with improper waste disposal, explaining, "Failing to dispose of waste, especially organic matter, attracts mosquitoes." She mentioned that not using air conditioning or screens on windows and doors allows mosquitoes to enter homes, adding, "Using AC or screens can significantly reduce the risk of mosquito intrusion."
Okusanya warned against engaging in outdoor activities during peak mosquito hours, such as dawn and dusk, which increases bite risk. "Being outdoors during these times makes you more susceptible to mosquito bites," she said. She also highlighted the importance of eliminating breeding sites, stating, "Failing to remove standing water from containers like flowerpots, tires, and bird baths allows mosquitoes to breed."
Furthermore, she noted that not using mosquito traps or repellents in outdoor areas can increase the risk of mosquito bites. "Utilizing traps or repellents in outdoor spaces is essential for reducing mosquito exposure," she added.
She further urged individuals to stay informed about disease outbreaks and take preventive measures, stressing, "Failing to stay informed and take action during outbreaks puts you at higher risk." By addressing these habits, individuals can significantly reduce their risk of contracting mosquito-borne diseases,” she added.
Prevention and Control Interventions of Mosquito-borne Diseases
Both malaria, dengue and yellow fever are spread by mosquitoes, and the prevention and control of these diseases heavily depend on vector control methods. Although for malaria, WHO recommends two key vector control interventions: insecticide-treated nets (ITNs) and indoor residual spraying (IRS). These methods have been effective in reducing the transmission of malaria, but their impact on dengue is limited due to differences in the behaviour of the mosquitoes that transmit the viruses according to WHO report.
Further more, the report shows that dengue-carrying mosquitoes, primarily Aedes aegypti and Aedes albopictus, are active during the day, making ITNs less effective. Instead, preventing dengue requires comprehensive strategies that include environmental management to eliminate mosquito breeding sites, the use of mosquito repellents, wearing protective clothing, and ensuring that homes have window screens or nets to keep mosquitoes out.
Currently, there is no specific antiviral treatment for yellow fever. WHO advises that patients should rest, stay hydrated, and seek medical advice. Treatment may vary depending on the severity of the disease; patients may be managed at home, referred for hospital care, or require emergency treatment. Managing dehydration, liver and kidney failure, and fever is crucial for improving patient outcomes. Additionally, associated bacterial infections can be treated with antibiotics.
Yellow fever is notoriously difficult to diagnose, especially in its early stages, as its symptoms overlap with other diseases such as malaria, leptospirosis, viral hepatitis, other hemorrhagic fevers, dengue, and even poisoning.
Polymerase chain reaction (PCR) testing of blood can sometimes detect the virus during the early stages, while later stages require testing for antibodies through enzyme-linked immunosorbent assay (ELISA) and plaque reduction neutralization test (PRNT) according to WHO report.
Okusanya emphasized the crucial role that proper sanitation plays in controlling and preventing mosquito-borne diseases. She pointed out that maintaining a clean environment is key to reducing the risk of these diseases. "Proper sanitation helps by eliminating mosquito breeding sites," she explained, noting that removing standing water and debris is essential in preventing mosquitoes from multiplying.

A vendor sells to customers in an unhygienic open drainage with stagnant water with risks of breeding mosquitoes in Ketu, Lagos State, Nigeria
She also highlighted that proper waste management and sanitation efforts lead to a decrease in mosquito populations, which in turn reduces the likelihood of disease transmission. "Regular cleaning and maintenance of drains, gutters, and containers prevent water stagnation, which is a major contributor to mosquito breeding," she added.
Okusanya stressed the importance of proper disposal of organic waste and debris, as it eliminates food sources for mosquitoes, further reducing their numbers. "A clean environment not only reduces mosquito-human contact but also prevents disease transmission," she said.
Moreover, she explained that these sanitation efforts enhance overall community health and well-being. "Sanitation is a key component of integrated pest management strategies, and it even helps reduce mosquito resistance to insecticides," she noted.

An aged woman who is a food vendor cooking in an unhygienic environment with contaminated stagnant water with risks of being exposed to mosquitoe bites in Wesley Close, Lagos State, Nigeria
She emphasized that proper sanitation is particularly important for protecting vulnerable populations, such as the elderly, children, and those with compromised immune systems. "By maintaining a clean and sanitary environment, we can significantly reduce the risk of mosquito-borne diseases and protect public health," she affirmed.
The Need for Equity and the Path Forward
WHO estimates that 80% of the global population is at risk of one or more vector-borne diseases. These diseases are not limited to malaria; mosquitoes, flies, bugs, and other vectors transmit a wide range of viruses, parasites, and bacteria that lead to deadly and debilitating conditions.
Vector-borne diseases thrive in conditions of poverty, where access to healthcare is often limited, and environmental conditions provide fertile breeding grounds for disease-carrying insects. The impact of these diseases is not only felt in terms of mortality but also in the long-term consequences for survivors who may be left permanently disabled or disfigured, further entrenching them in cycles of poverty and disadvantage.
Economically, these diseases place a heavy toll on affected communities, restricting both rural and urban development.
Urbanization, especially unplanned urban growth, has also contributed to the spread by creating environments conducive to mosquito breeding. High population density, inadequate waste management, and unreliable water sources increase the risk of transmission. Community knowledge, attitudes, and practices towards disease prevention are crucial in controlling the spread of these diseases.
By investing in vector control, enhancing community awareness, and improving access to healthcare, the world can make significant strides toward reducing the burden of malaria and dengue.
This fight is not just about controlling diseases; it is about achieving health equity, promoting sustainable development, and protecting the future of communities around the world.
Source : Lead News Online
Author : Collins Odigie Ojiehanor/Lead News Online's Special Report Contributor
The author is a Health and Environmental reporter based in Lagos, Nigeria.