Oropouche: The mysterious 'sloth virus' with no treatment

A mysterious virus once confined to the Amazon is now spreading more widely around the Americas, after undergoing genetic changes that may make it more potent.
Until recently, Oropouche virus was a relatively-unknown disease largely confined to within the Amazon basin in South America. But since late-2023, the virus has been spreading beyond its usual range.
It has already caused more than 8,000 cases of the disease – often known by its nickname "sloth fever" – in five countries during the first seven months of 2024. The virus also recently caused the deaths of two women in Brazil and the potential deaths of two unborn children.
The rapid increase in cases of Oropouche, which is spread by biting insects, led the United States Centers for Disease Control and Prevention (CDC) to issue a health advisory alert to doctors in the US. The first cases of the virus in Europe were detected in June and July 2024 in travellers who had been infected while visiting Brazil and Cuba.
What is this mysterious virus, where did it come from and why is it causing concern?
What is Oropouche virus?
Oropouche is a virus endemic to the Amazon region of South America that is spread by biting insects.
The virus causes a feverish disease in humans but is also found in a number of animals including howler monkeys, marmosets and sloths, along with a number of different insects.
How does the virus spread?
Oropouche is transmitted when a person or animal is bitten by insects carrying the virus. It is thought to be spread most commonly by the pinhead-sized midge species Culicoides paraensis, which are abundant across large parts of the Americas. But the virus may also be spread through bites by the Culex quinquefasciatus and Ochlerotatus serratus mosquitoes.
Direct human-to-human transmission of the virus has not been observed.
Once in the blood stream it can quickly spread around the body, and can cross the blood-brain barrier to get into the central nervous system. It appears to particularly accumulate within both the brain and liver.
Where does Oropouche come from?
The virus gets its name from the village where the first case was recorded. In 1955, the virus was isolated from the blood of a feverish 24-year-old forest worker in the community of Vega de Oropouche in Trinidad and Tobago.
Since then, the virus has been responsible for sporadic outbreaks across the Brazilian Amazon, with some reported to reached up to 100,000 cases. In total, researchers estimate that more than 500,000 cases have been diagnosed, but this number may be an underestimate due to misdiagnosis, as many of the symptoms are similar to other fever-causing illnesses.
From the late-1980s, outbreaks of the virus began to be reported in Panama, Peru and Ecuador. But since 2000, the number of countries reporting the virus has increased to include Bolivia, Colombia, Ecuador and French Guiana.
In late-2023, large outbreaks began to occur in the Amazon basin, where the virus was already endemic, and in new areas of South America. In June 2024, Cuba confirmed cases of the virus.
Between 1 January and 20 July 2024, the World Health Organization recorded 8,078 cases of Oropouche. The majority – 7,284 including the two deaths – were in Brazil, with Bolivia recording 356, Peru reported 290, Colombia with 74 and Cuba with 74.
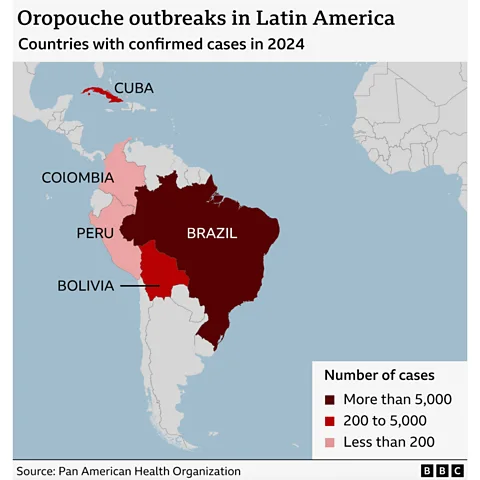
Most worryingly for public health officials, a growing number of cases are now occurring in non-Amazonian areas, and they have been documented in 10 states outside of the Amazon region in Brazil, as well as Cuba.
Recent unpublished analysis of the virus behind the latest outbreaks suggests its genetic code has undergone some reshuffling that led to it replicating more efficiently in the cells of infected individuals. This means the virus can produce far higher numbers of itself once it infects a cell and hijacks the cellular machinery.
This would not only allow the virus to potentially cause more severe disease in infected individuals, it also increases the chances of biting insects picking up the virus when feeding and passing it on.
While the virus's ability to hide within immune cells means it could remain relatively hidden from the body's defence system, there are some signs the virus may be more resistant to the immune response of people previously infected with Oropouche.
Scientists also believe that increased urban development into areas that were once forest may also be playing a role in the new outbreaks. They say that the effects of climate change are increasing the number of areas where the insects that spread the virus can live, meaning the virus is likely to continue expanding beyond its historic range in South America.
What are the symptoms of Oropouche?
The virus causes a flu-like fever in infected people, along with a headache, muscle aches, stiff joints, nausea, chills, sensitivity to light and vomiting. In severe cases it can cause meningitis. In general, the symptoms are similar to other mosquito-borne diseases like dengue, chikungunya, Zika and malaria.
According to the CDC, symptoms typically start three to 10 days after being bitten and last for three to six days. Symptoms can reoccur a few days or weeks later in up to 60% of patients, and tend to be similar on relapse. It is not clear what causes these relapses; it could be the same infection re-emerging, or people living in areas with a high prevalence of virus-carrying insects being re-infected.
How deadly is Oropouche fever?
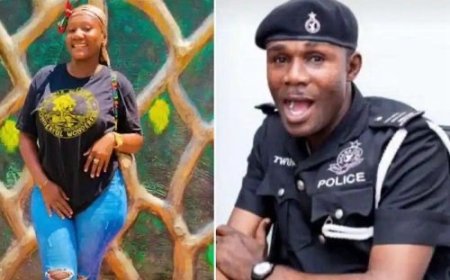
On 25 July, authorities in Brazil recorded the known first deaths from Oropouche fever. The two women were aged 21-years-old and 24-years-old, with neither having any pre-existing health conditions.
A report by the Brazilian Ministry of Health has also suggested that the virus could be transmitted from pregnant women to their foetuses, and reported the death of one unborn child. It has also reported a miscarriage associated with Oropouche infection. Four cases of newborns with microcephaly – a birth defect where the baby's head is smaller than expected – were also reported to be associated with the virus.
However, the effects of Oropouche on pregnancies and unborn children remains unproven and is being investigated.

Why is it known as sloth fever?
While the first wild animals found to carry the virus were howler monkeys, in 1960 it was also isolated from a pale-throated sloth in Brazil.
However, a number of other wild animals are also thought to carry the virus. And the main wild host of the virus has yet to be identified.
What treatment is available?
An article in the academic journal The Lancet Microbe classifies outbreaks of Oropouche fever as "an emerging threat to global health" and warns of the lack of research into new treatments.
Other researchers have underlined the "urgent need for effective vaccines" against Oropouche. While vaccines are being tested in animal models, there aren't any yet available or known to be effective in humans.
There are currently no specific treatments for the disease.
Brazil's Ministry of Health says that "patients must rest, with symptomatic treatment and medical monitoring".
Anyone infected should also continue to use insect repellents, to reduce the likelihood of their being bitten by insects, which could then transmit the virus to other people.
Can Oropouche be prevented?
Without vaccines to control infections, the best way people can protect themselves against Oropouche is to avoid being bitten by midges and mosquitoes. Health authorities suggest using fine mesh nets on doors and windows. As the midge that carries the disease is smaller than mosquitoes, standard mosquito nets are thought to be less effective.
Wearing clothing that covers arms and legs and using insect repellents can also help to protect against bites.
Source: BBC